Body mass index may not be the best indicator of our health – how can we improve it?
- 30 July 2020
By Dr Karen Coulman, Research Fellow (NIHR Clinical Lectureship), and Dr Sarah Sauchelli Toran, Senior Research Associate, at the University of Bristol and the NIHR Bristol BRC Nutrition, Diet and Lifestyle theme.
Their article was originally published in The Conversation, 29 July 2020.
Body mass index or BMI has long been the standard for measuring health. The simple formula is widely used to classify whether our weight falls within a “healthy” range for our height. BMI provides an estimate of a person’s overall disease risk, and is used around the world to measure obesity.
But BMI has come under criticism because it can be inaccurate in estimating body fat and doesn’t provide a full picture of a person’s health. Research also shows that relying on BMI alone to predict a person’s risk of health problems can be misleading.
The formula for calculating BMI was first invented in 1832 by Belgian mathematician and astronomer Adolphe Quetelet. To calculate it, you divide weight in kilograms by height in metres squared (kg/m2). In adults, BMI is categorised as follows:
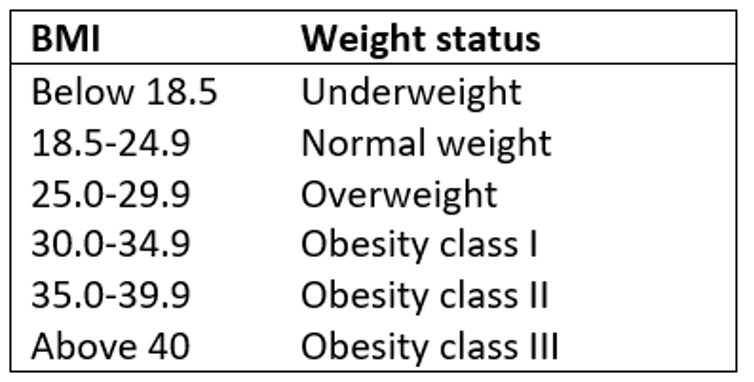
BMI categories to define weight status. Sarah Sauchelli Toran and Karen Coulman, Author provided
BMI is a quick, easy, and cheap way of diagnosing overweight or obesity needing only a weight and height measurement. Since obesity carries an increased risk of disease, including heart disease, stroke, and diabetes, BMI can identify those at greater risk of developing health problems. It’s also sometimes used to make decisions about who gets certain treatments, and to evaluate how effective certain weight loss interventions are.
But BMI alone doesn’t give a full picture of a person’s health risk, as it’s simply a measure of body size – not of disease or health. BMI doesn’t actually measure body fat, a key element when establishing health risk. Although it provides a rough indication of body fat, it doesn’t distinguish between weight coming from fat versus muscle.
High-performance athletes – such as rugby players or sprinters – would be classified as “overweight” or “obese” by their BMI because of their greater muscle mass. Looking at BMI alone would make it appear athletes are at a similar risk of the same health problems as someone who’s overweight – even though research shows active people have better cholesterol, blood pressure, and lower blood sugar levels than someone who’s inactive.
BMI also doesn’t tell us anything about where body fat is distributed. Body fat stored around the abdomen (an “apple” shape) poses a greater health risk than body fat stored around the hips. This “apple” shape is associated with an increased likelihood of developing metabolic syndrome. This is a combination of related conditions – such as high blood pressure, high blood glucose, and high cholesterol levels – all of which increase the risk of heart disease, stroke and type 2 diabetes.
BMI categories are also somewhat arbitrary. A study of 13,601 adults showed the prevalence of obesity was much lower when defining obesity using BMI instead of body fat percentage. Using BMI categories, less people were found to have obesity – though many would have been diagnosed as such because of their body fat percentage.
These categories may be even less accurate in predicting health risks in people from ethnic minority backgrounds and older age groups. For example, Asian people are at greater risk of developing type 2 diabetes and heart disease at lower BMIs than Caucasian people. This may be due to a higher body fat percentage at similar BMIs, and/or a greater tendency to store fat around the abdomen.
Research also shows that in adults aged 65 and over, having a BMI within the “overweight” category wasn’t associated with a greater risk of death whereas a BMI below 23 was. So normal ranges may not work well for predicting health risks in older people.
People can also have a “normal” BMI but have an increased risk of heart disease and type 2 diabetes, depending on factors such as their blood pressure or body fat distribution. Measuring waist circumference and body fat percentage may be more useful in such cases.
Reliable, affordable and accurate indicators of health status are important. BMI is easy to measure and provides a rough estimate of disease risk. But while it’s a good starting point, BMI needs to be used alongside other measurements to get a fuller picture of a person’s unique health risk. Lifestyle factors (such as smoking, physical activity, diet and stress levels), and blood pressure, blood sugar and blood cholesterol levels should all be considered alongside BMI to establish health risk.
Waist measurements (such as waist circumference and waist-to-hip ratio) can estimate abdominal body fat – but they can be difficult to undertake and less accurate in people with a BMI higher than 35. Tools that break down body composition – such as bioelectrical impedance analysis and dual-energy X-ray absorptiometry – work better. But these can be very expensive, time-consuming and complex to use – and wouldn’t be practical for everyday use by GPs.
Staging tools may provide a more tailored assessment of health risk and early death in people living with obesity. These are scoring systems which take into account metabolic, physical and psychological health to classify health risk. They’re designed to be used alongside BMI to identify people who would benefit most from weight management interventions.
While BMI provides a convenient and simple tool for understanding disease risk, it doesn’t provide a full or entirely accurate picture of everything that influences our health. Using other measurement tools alongside BMI can provide a more complete picture of health and disease risk – and may also help guide decisions about the best health interventions to use for a specific person.